After receiving treatment for a life-changing traumatic event or diagnosis in a traditional children’s hospital, where do children go before returning home? After all, their recovery journey doesn’t end once they exit those hospital doors.
Next steps after intensive care can be daunting. Families are left scrambling, unsure of what options are available, and unaware of the resources that could support them. And, many hospitals and providers don’t know what happens to these kids once they leave their care.
For years, I’ve been working to identify the gaps that exist in the continuum of care for medically-complex kids. The goal is to help families and healthcare providers nationwide understand the resources available, and how to provide the best post-acute care.

Recent Research Helps Identify Resources – and Gaps
Recently, a paper published in Pediatric Critical Care Medicine by a group of pediatric intensivists from Boston Children’s Hospital (a training and research hospital of Harvard Medical School) brought some much-needed attention to the issue.
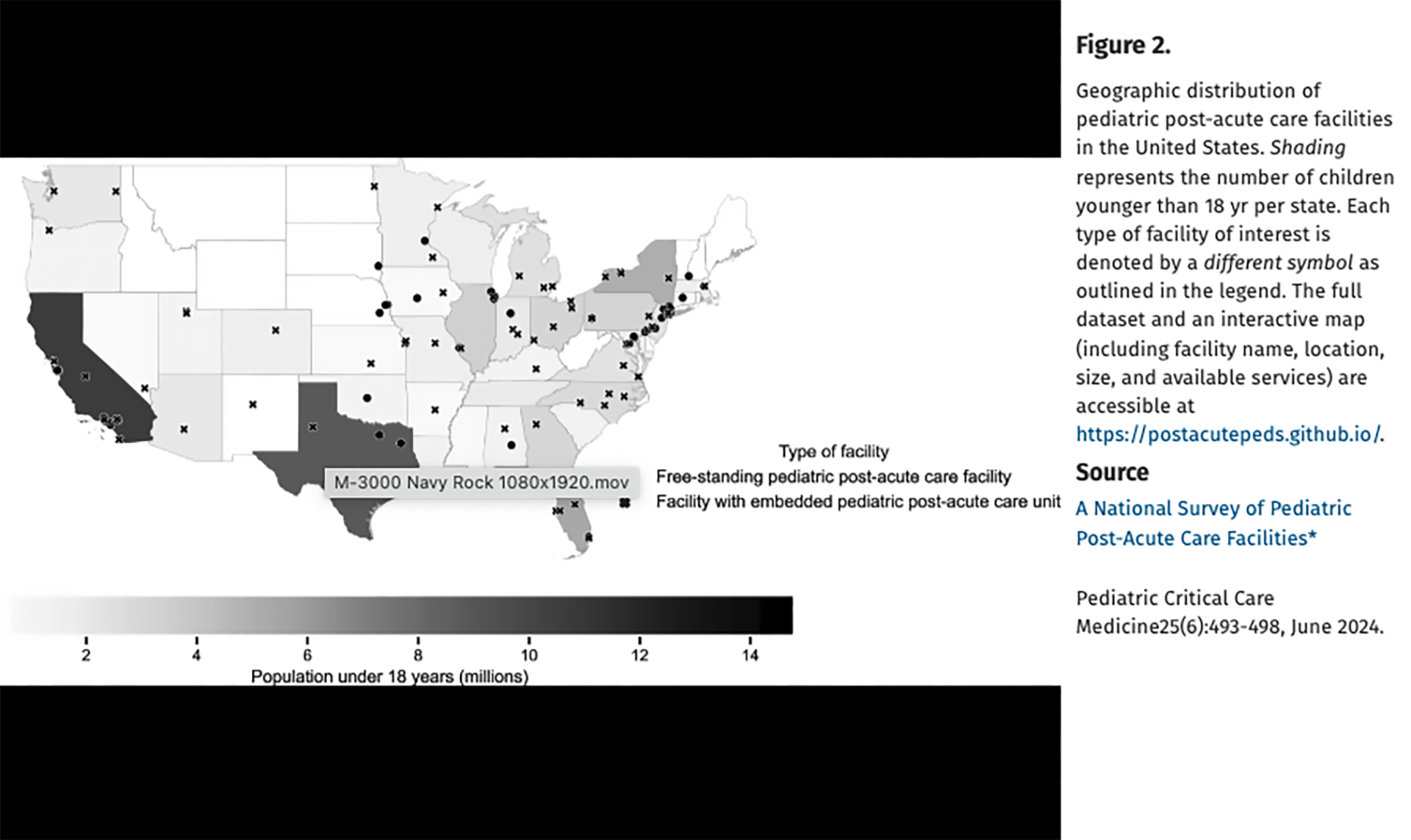
The study – focused on care options for high-needs children – highlighted 109 facilities across the country where post-acute care resources are available, and eye-opening information on where they are missing. In primarily rural areas and 11 entire states, there are not any post-acute care facilities or programs dedicated to pediatric care.
The research also found that families and healthcare providers are unaware of post-hospitalization options, and how limited bed availability often delays care.
This study was a major step forward for our industry, but there is still work to be done. Unfortunately, many facilities that provide post-acute pediatric care were not included in this research. But even taking those into account, there are swaths of our country that simply don’t have any options for this kind of care.
These children often require ongoing care and support, but the current system has large blind spots, making it difficult for families to access critical information about post-acute care facilities.
The Hurdles of Awareness and Resource Mapping
Over the past few years, I’ve been working with fellow complex care practitioners and a greater team to collect data from other institutions and information that can help identify the missing pieces.
Together, we are working on creating a survey to send to hospitals, aiming to gather detailed information about post-acute care services.
The goal is to build a comprehensive directory of institutions, programs and caregivers that will connect children and families managing complex medical conditions with the help they need.
Why This Matters: The Growing Population of Medically Complex Kids
The number of children with medical complexity is growing, and their needs are significant.
Yet, the pediatric healthcare system is not equipped to fully support them due to a lack of post-acute care resources. Families often struggle under the immense stress of caring for a child with complex needs.
Many families face readmissions soon after discharge because they lack the support necessary to keep their child stable at home.
A directory of post-acute care resources would serve as a lifeline for families and healthcare providers alike, allowing them to navigate the often fragmented system of post-acute care.
And, it will allow for better collaboration between medical providers in the U.S. to address the needs for complex patients.

Healthcare Providers: Help Us Bridge the Gaps
The pediatric medical community has made strides in understanding and addressing post-acute care needs, but there is still much work to be done.
Mutual awareness among healthcare providers and facilities is essential for collaboration and improvement.
As the study shows, it’s possible to collect and compare information across the country, but it will take continued efforts to close the gaps in pediatric post-acute care. There needs to be more studies like this one that look into what pediatric post-acute care options are available and where. There also needs to be more studies done on children’s experiences in those facilities, like Ranken Jordan’s recent time-motion study.
The time is now for the medical community to collaborate and make sure that no family is left to navigate their unique and challenging journey alone.
E-Newsletter Coming Soon!
Sign up today to subscribe and receive our upcoming e-newsletter.






