This is an article written by Duha Al-Zubeidi, MD, and Melanie Hubert, RN, for the Pediatrics Complex Care Association (PCCA).
The biggest threat across the country as we continue to see a steady rise in COVID-19 cases is what we may face in just a few months—Influenza. The 2019-2020 Influenza season was one of the most severe in recent years; the CDC reported more than 50,000,000 flu illnesses, 740,000 flu hospitalizations and 62,000 flu deaths. Of those, 188 were pediatric deaths [1]. As of August 25, COVID-19 has affected more than 5.7 million in the U.S. alone, with more than 178,000 deaths. Of those, 92 were pediatric deaths [1,2,3]. Despite the large number of COVID-19 cases both in the U.S and worldwide, there’s a lot we still don’t know about COVID-19. Evidence so far suggests that children with medical complexity (CMC) are at increased risk for severe illness and therefore our continued attention to this topic is of high value [4].
We already know that influenza tends to be severe in CMC and can have devastating outcomes in this population. A study looking at CMC in an inpatient setting found that respiratory tract infections were among the most common infections. Influenza was a major contributor to residents’ illnesses and outbreaks. This was despite residents of these facilities having an influenza vaccination rate of greater than 90% (good job PCCA!). Of staff working in these settings, there was a lower, variable rate of vaccination of 75-99% [5].
It’s important to educate staff and patients that the flu shot works especially in the pediatric population. The CDC reported that 75-80% of children who die annually with influenza are unimmunized, although the vaccines’ overall effectiveness may appear low to the public (VE: 45-55%) (6). The time is now: Getting a Flu shot may be more important this season than ever before. Not only will this provide protection from influenza, it will reduce symptoms that might be confused with those of COVID-19, alleviating continued stress on the health system. The CDC advisory committee of communication practices (ACIP) published updated recommendations for this upcoming season (7). The vaccine will have very similar components to last year. This year, the flu mist is also available. The American Academy of Pediatrics has not preferred one vaccine over the other.
As health care providers, we must educate our patients, their families, our co-workers and others on common misconceptions regarding a flu shot: The vaccine does not give you the flu. The vaccine is still safe for individuals with egg allergy. Getting a flu shot does not make you more vulnerable to contracting COVID-19. There is no part of COVID-19 integrated into flu vaccine. The ACIP does recommend waiting to get well if you are infected with COVID-19 before you get an influenza vaccine (7).
Here are 8 tips to help your facility prepare for the 2020-2021 Flu Season:
- Start your influenza campaign earlier this year, a socially distanced influenza administration protocol will take planning ahead. Be creative—outdoor booths, and drive thru vaccination, rather than gathering in one room or lining up to get the vaccine. Offer vaccination to families as well, as they may not be able to or want to visit their usual health care providers because of COVID-19.
- Plan for employee vaccination to occur by mid-late September and by Halloween for your patients. Don’t give it too early becauseimmunity can wane and lead to suboptimal protection later in the season.
- There are very few contraindications for the vaccine. Look very carefully at those employees or patients who refuse a flu shot or ask for a medical exemption. Look at the big picture and think of this as one pandemic you can control, help with and have an impact on.
- Continue to restrict visitation and traffic into your facility. This may mean your institution will continue to restrict visitors or only allow 1-2 designated visitors for the length of hospitalization. It may mean children have less indoor recreational activities or fewer indoor community integration opportunities. Be creative! Think about incorporating outdoor activities. (At Ranken Jordan our patients are enjoying fishing trips!). This is what it will take to protect our children.
- Everyone needs to be wearing a mask by now when in the hospital and adding on eye protection when interacting with patients particularly those patients who are unmasked or when interacting with unmasked visitors. All patients who are able to mask, should have a mask available to them, and encouraged to wear them when interacting with others. The Southern hemisphere is reporting unusually low influenza activity this season. This is being attributed to universal masking, continued lockdown, and restricted travel in addition to high influenza vaccination rates.
- Staff should continue to be self-aware and extra careful when in break rooms or when interacting with each other. Many reported COVID-19 outbreaks among healthcare workers in healthcare facilities have been traced back to times when they let their guard down and removed their mask—including breakrooms, during pot locks, or while socializing at the nurses’ station or residents’ lounges.
- As we start seeing symptoms, we need to stress the importance of staff not coming to work sick, even if it seems minor or something as insignificant as a cough. Look and see if your facilities’ culture promotes Presenteeism. If it does, what can be done to change this? If you are sick, this is the year to stay home and take care of yourself. By doing so, you are taking care of your patients and co-workers. Most employee outbreaks can be traced back to a single employee who either had a mild symptom they ignored or came to work knowing they were sick because they were concerned about “getting into trouble”. These behaviors end up infecting many more in the long run.
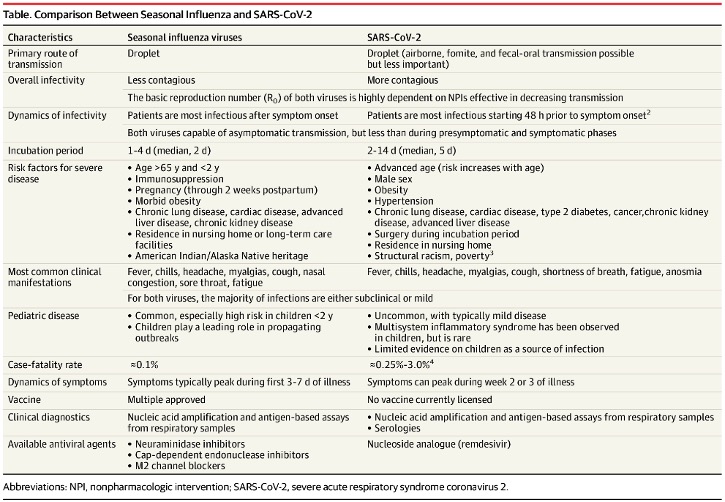
- It will be impossible to differentiate influenza disease from COVID-19 without adequate testing as symptoms for sure overlap (see table). Early identification of type of illness is key to implementing appropriate infection control measures. Antiviral treatment for influenza within 48 hours decreases morbidity and mortality and more so for our vulnerable population. During influenza outbreaks, antiviral chemoprophylaxis should be provided to all residents of institutional facilities (e.g., nursing homes and long-term- care facilities), regardless of vaccination status.
Be safe and stay in touch! (while practicing social distancing, Universal Masking, eye protection and hand hygiene, of course)
Table: Comparison Between Seasonal Influenza and SARS-CoV-2 (8)
References
- Burden of influenza. CDC. Published April 17, 2020. Accessed August 25,2020. https://www.cdc.gov/flu/about/burden/index.html
- New York Times. Coronavirus in the U.S.: latest map and case count. Retrieved from: https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html. Last accessed August 25,2020
- Children and COVID-19: State Data Report A joint report from the American Academy of Pediatrics and the Children’s Hospital Association Summary of publicly reported data from 49 states, NYC, DC, PR, and GU Version: 8/20/20
- Kim L, Whitaker M, O’Halloran A, et al. Hospitalization Rates and Characteristics of Children Aged <18 Years Hospitalized with Laboratory-Confirmed COVID-19 – COVID-NET, 14 States, March 1-July 25, 2020. MMWR.
- Saiman L, Maykowski P, Murray M. Incidence, risks, and types of infections in pediatric long-term care facilities. JAMA Pediatr. 2017;171:872–878.
- S. Flu VE Data for 2019-2020. Description of patients enrolled in the US FLU VE network, 2019-2020. https://www.cdc.gov/flu/vaccines-work/2019-2020.html
- Centers for Disease Control and Prevention (CDC): Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2020-21 Influenza SeasonMMWR Morb Mortal Wkly Rep.; August 21, 2020;69(RR-8);1-24.
- Solomon DA, Sherman AC, Kanjilal S. Influenza in the COVID-19 Era. Published online August 14, 2020. doi:10.1001/jama.2020.14661